Practice Management
At MedConnectHealth, we know the importance of healthcare providers getting paid in a timely manner! That’s why our practice management tools make it easier for providers to do what they do best!
Practice Management
At MedConnectHealth, we know the importance of healthcare providers getting paid in a timely manner! That’s why our practice management tools make it easier for providers to do what they do best!
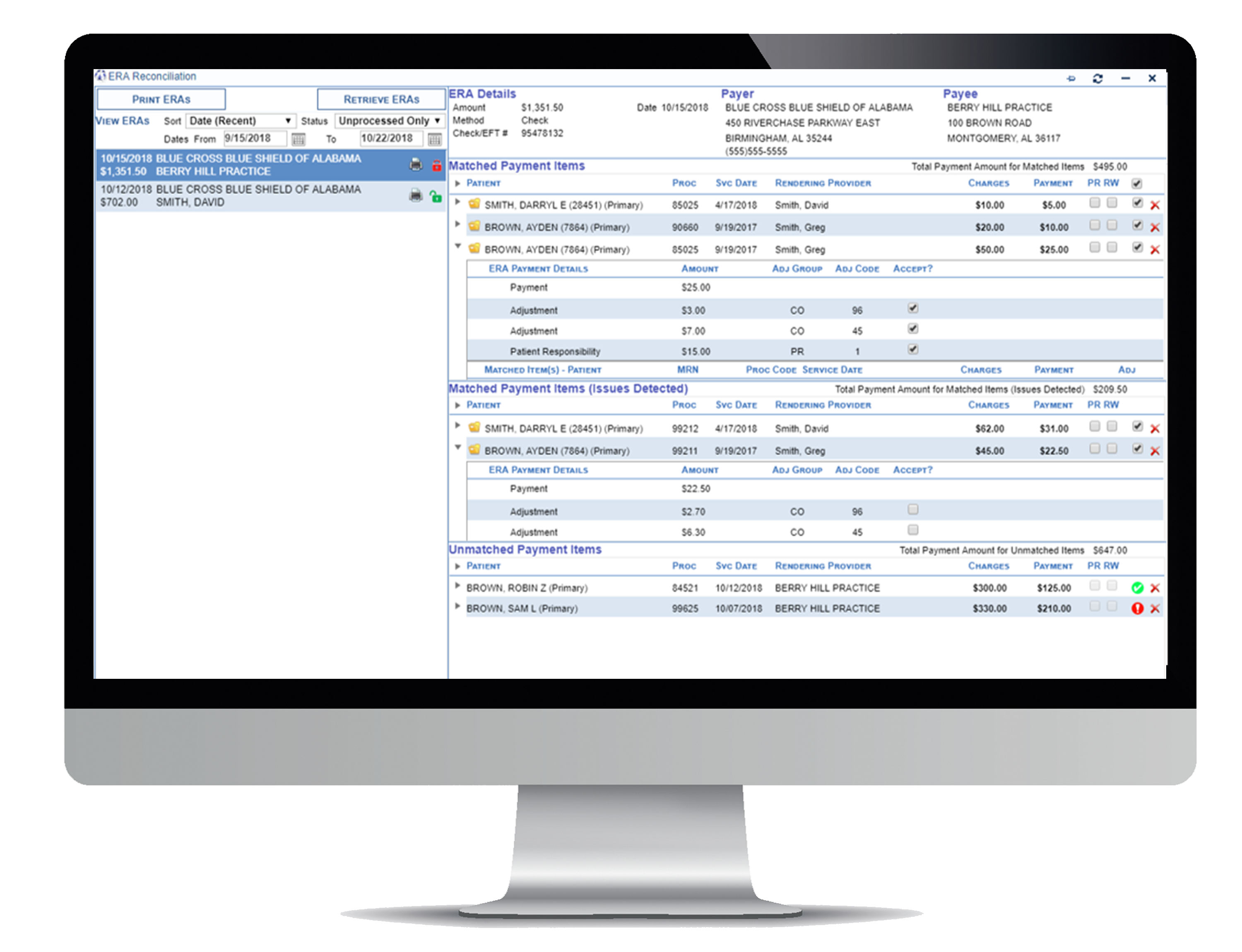
MedConnectHealth makes claims management easy by performing the following:
- Charges are categorized by Pending Processing, Submission, and Rework
- Quickly review, validate and process charges in dashboard
- Generate electronic claims and/or paper claims
- Transmit claims through ClaimMD, Change Healthcare, Trizetto, and Waystar
- Direct claims submission to Blue Cross/Blue Shield of Alabama
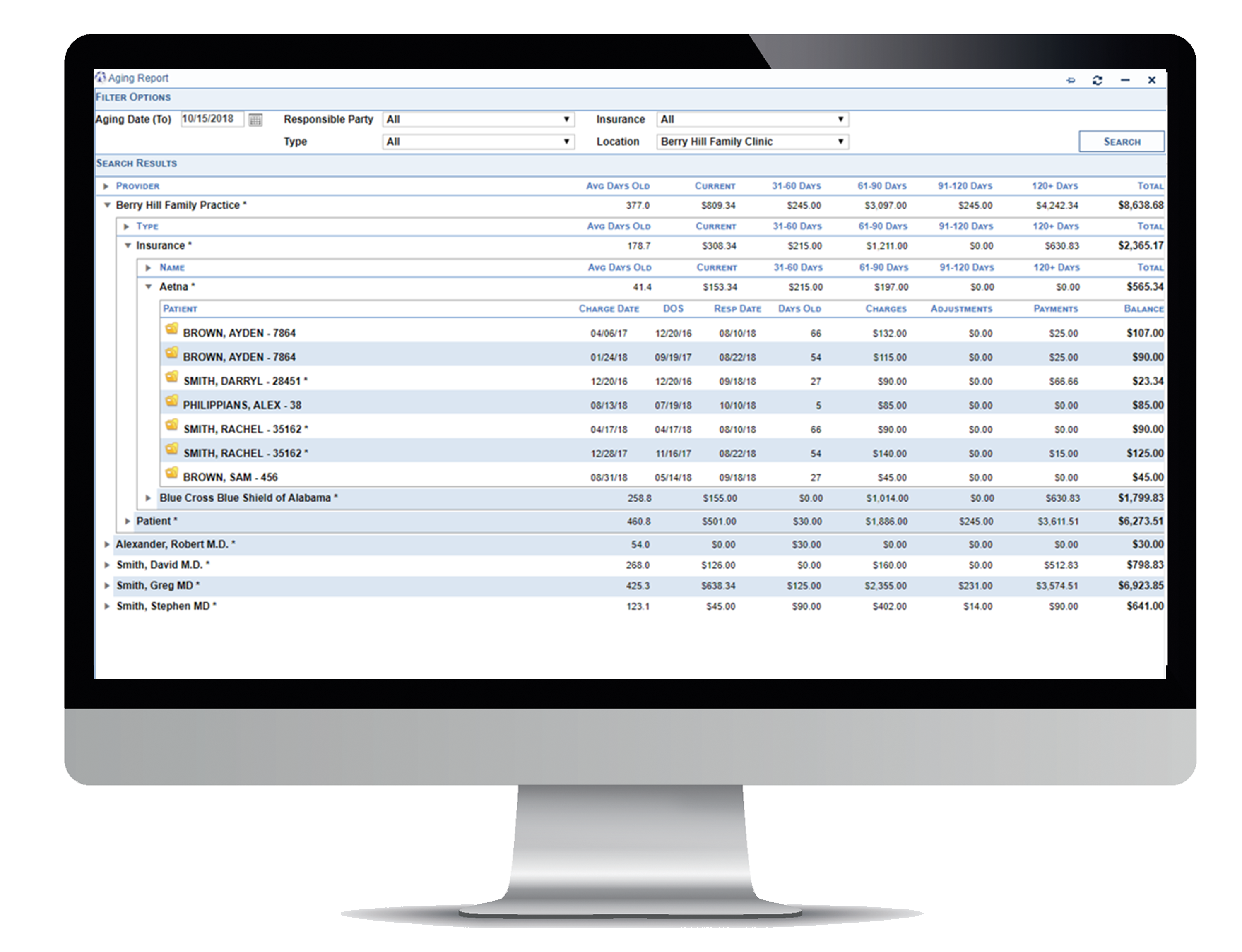
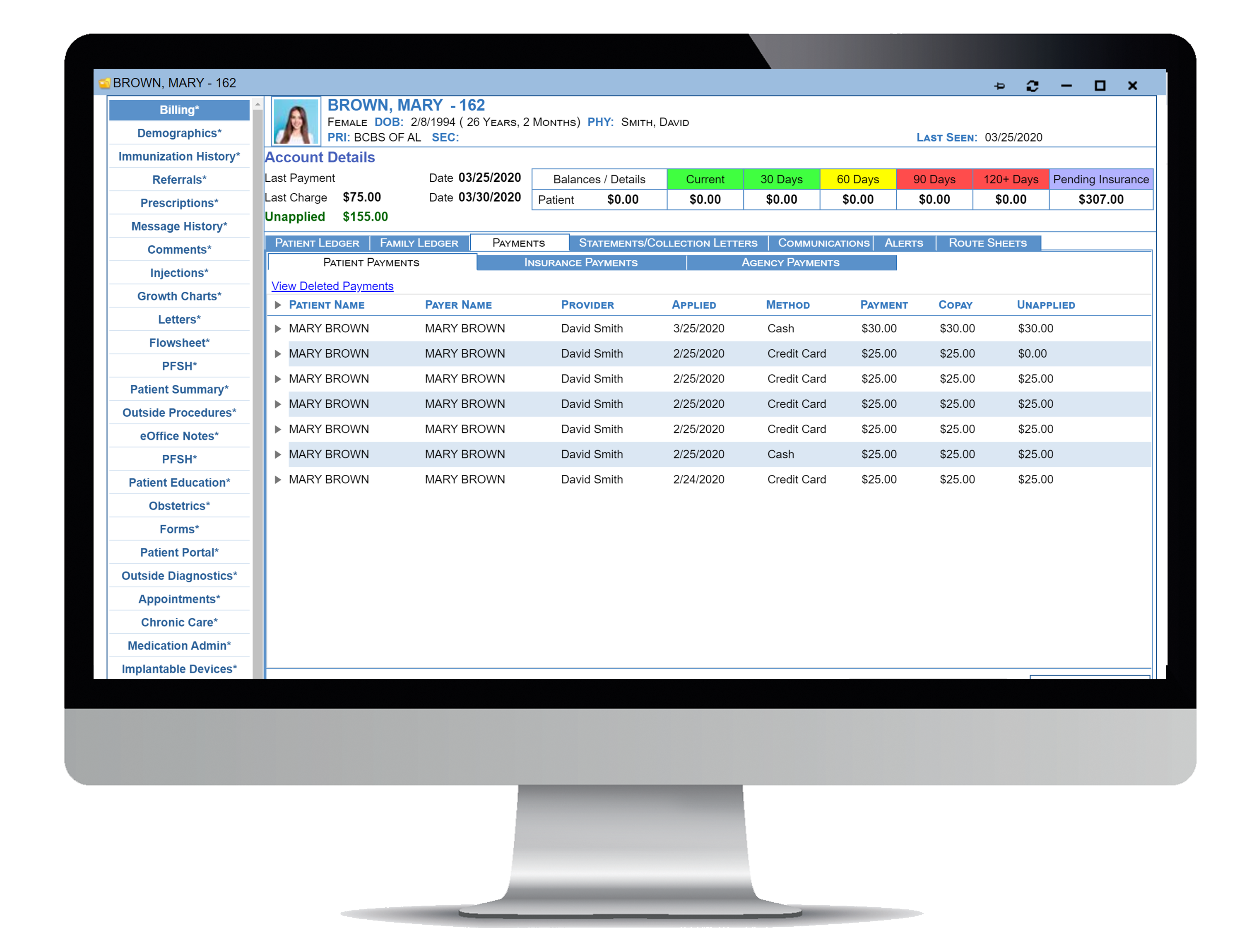
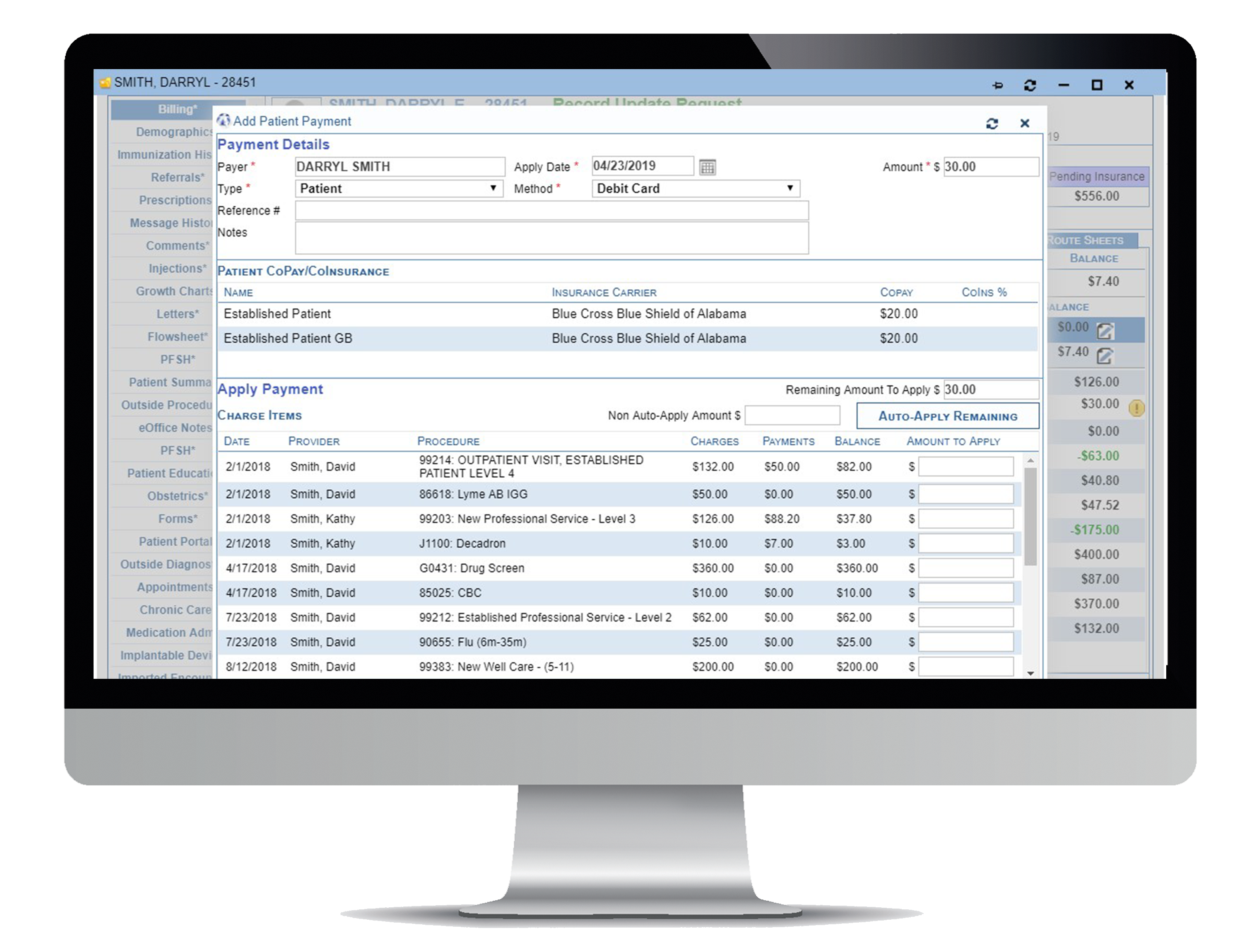
Payment processing could not be any easier with MedConnectHealth:
- Automatic downloading of electronic remittances
- Validation of received payments before posting electronic remittances
- Post manual payment checks and apply to outstanding charge items
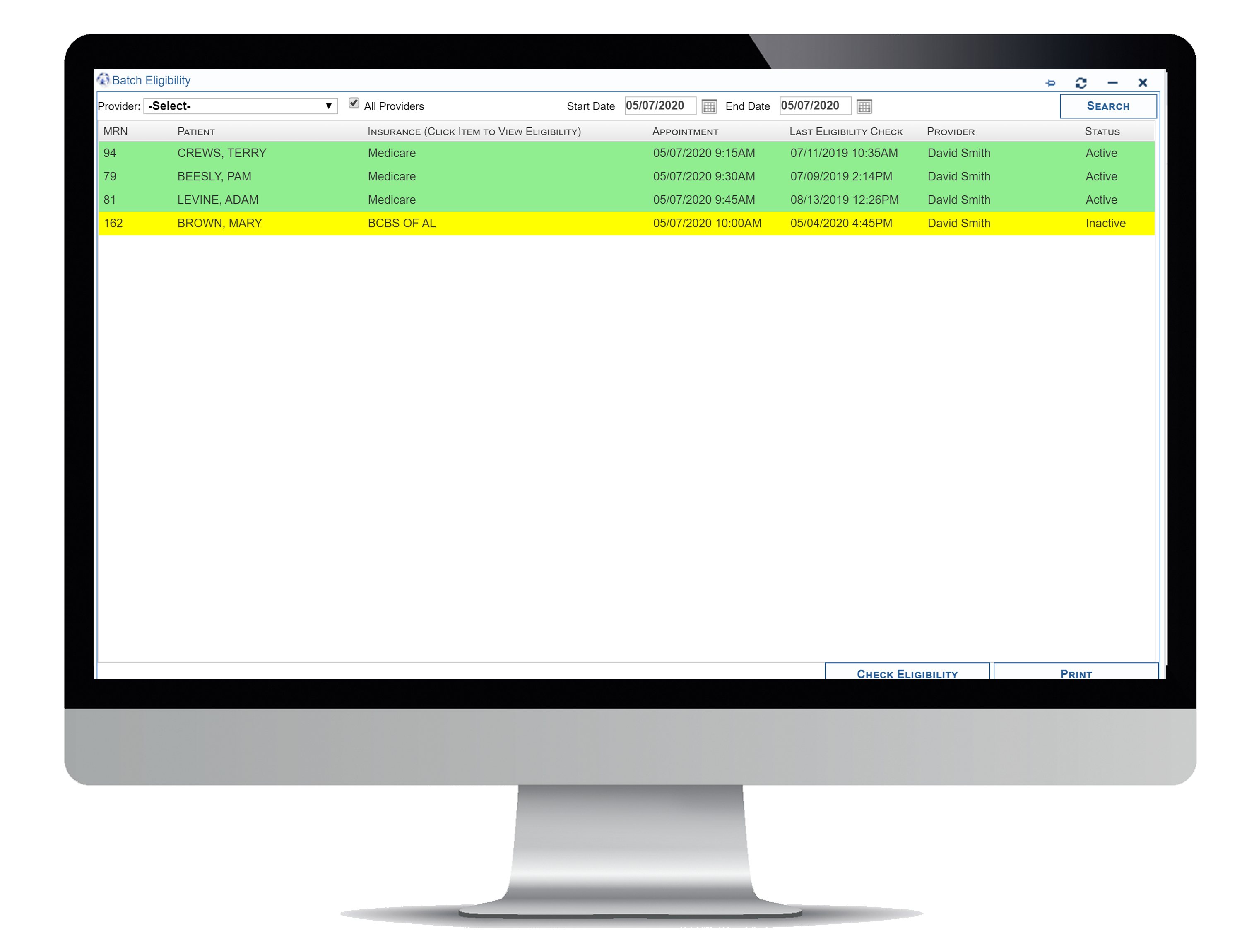
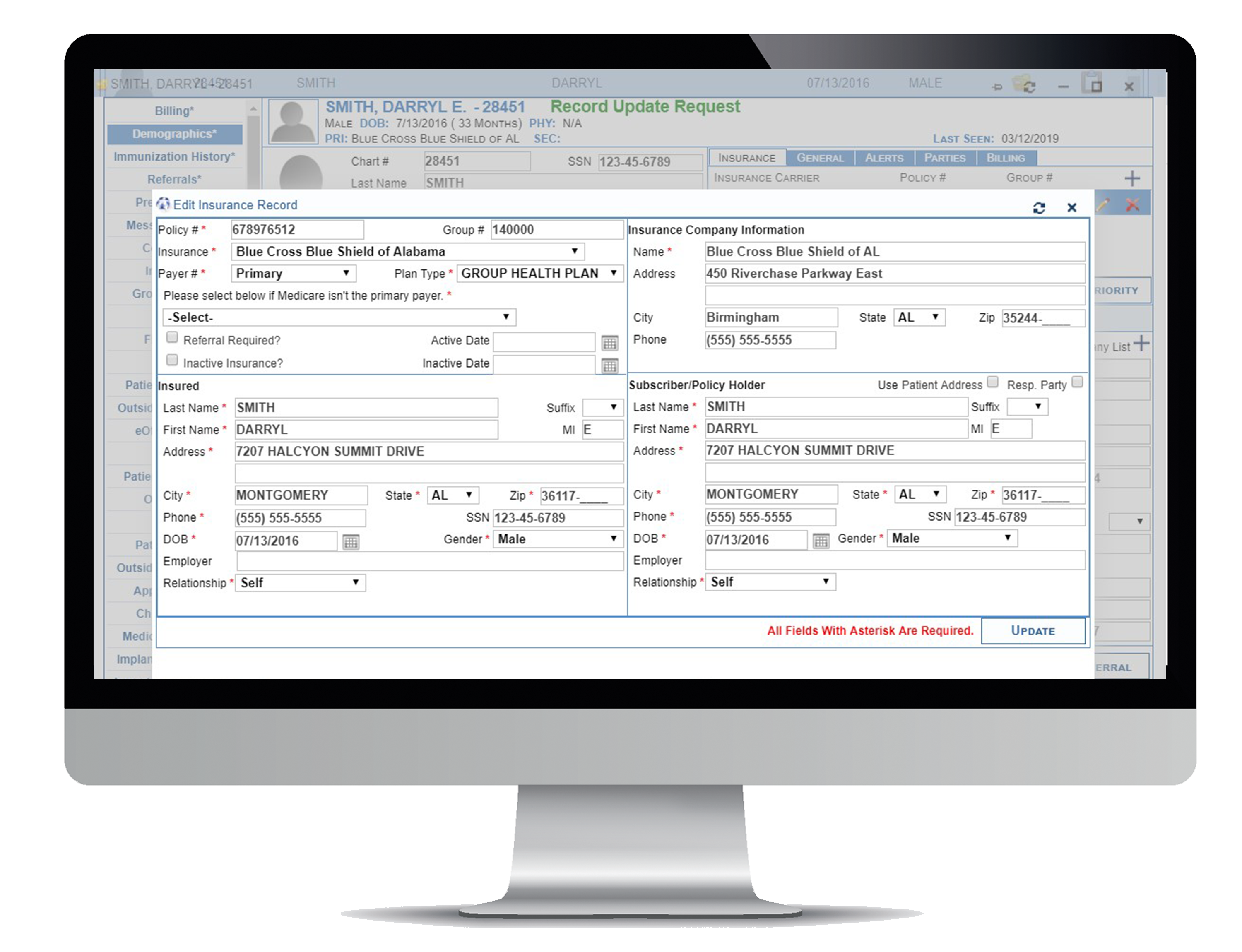
MedConnectHealth helps better inform you on insurance eligibility and benefits:
- The ability to check insurance eligibility and benefit details for patient’s insurance plans. Insurance eligibility can be performed from the schedule and the patient’s chart.
- Perform batch eligibility
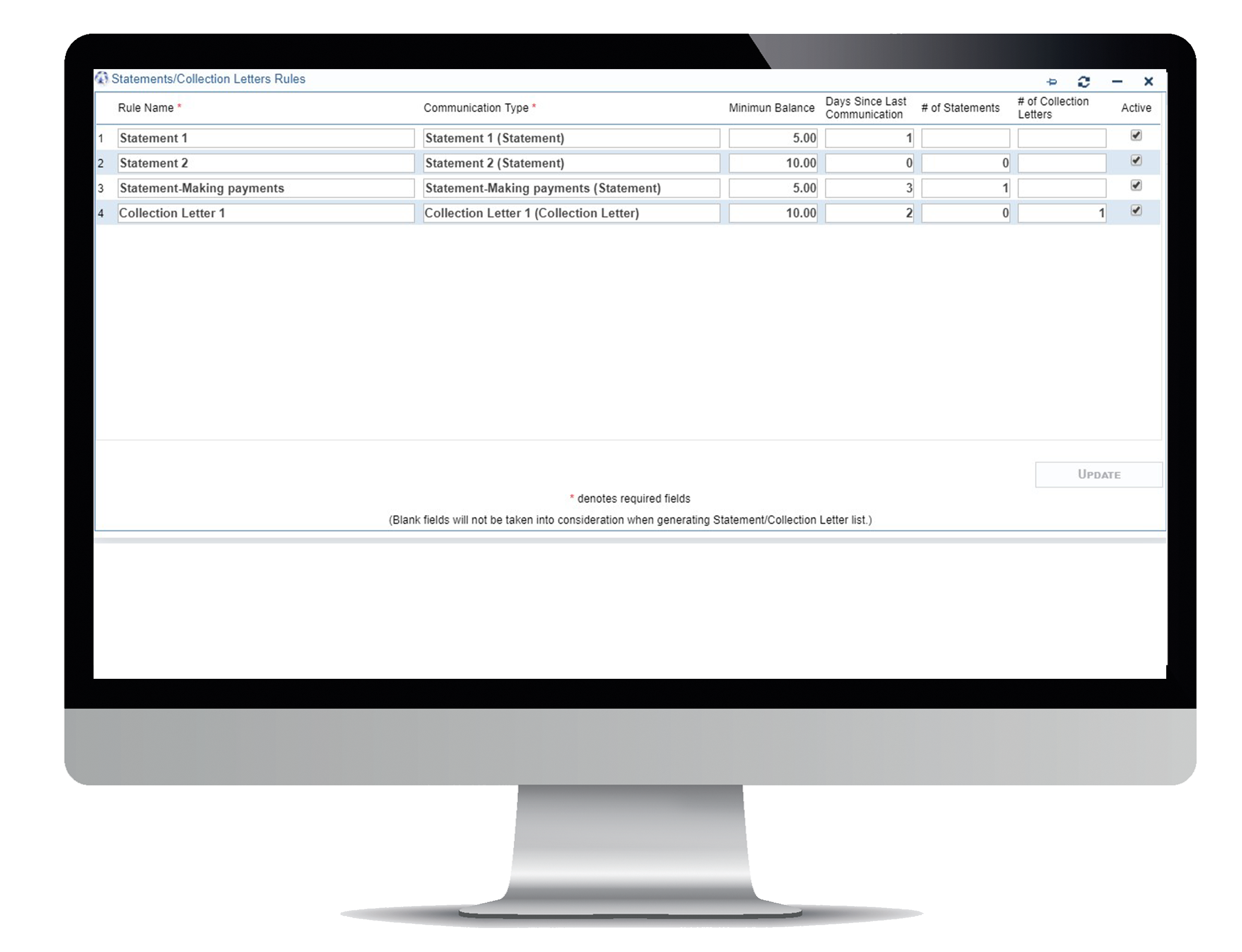
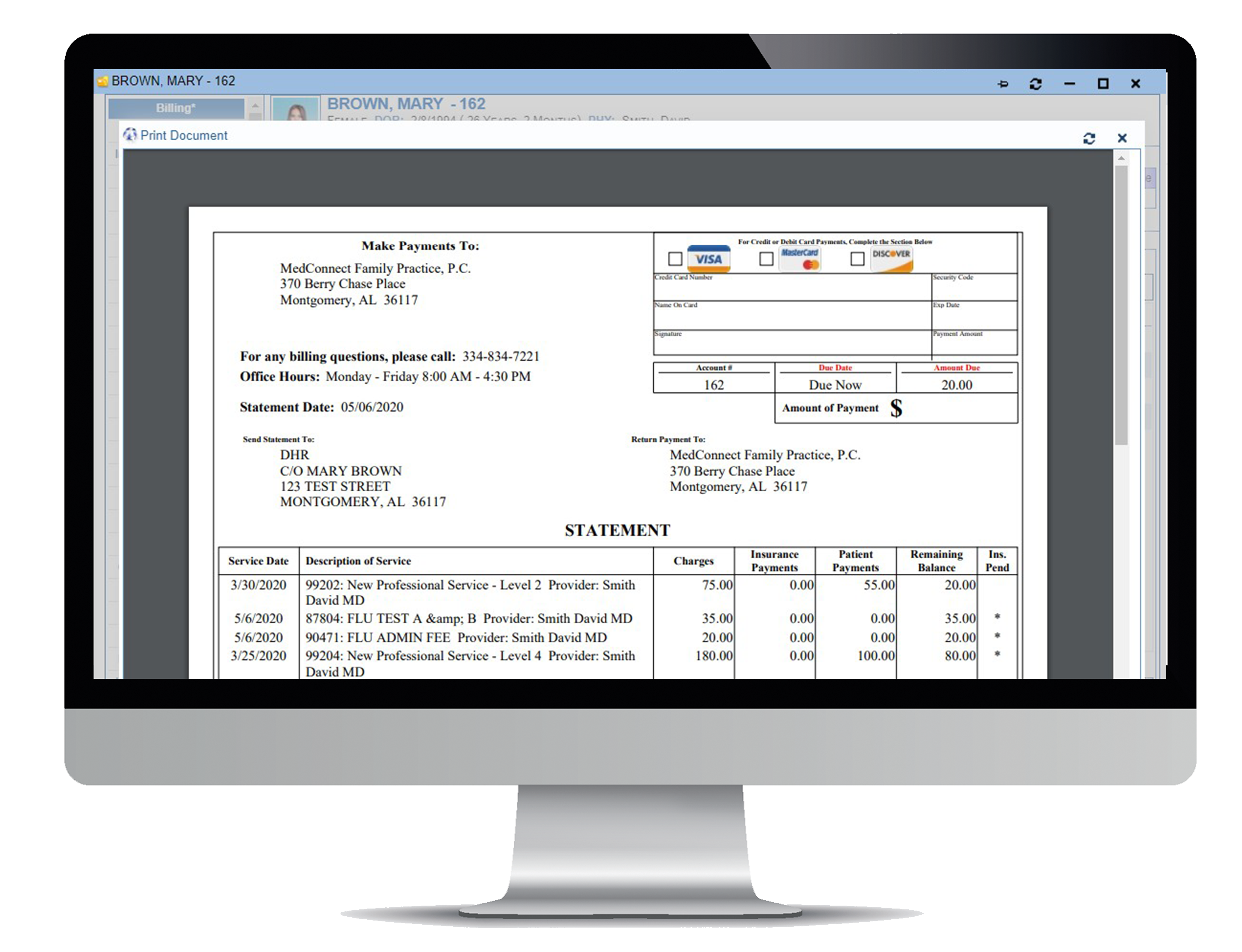
MedConnectHealth simplifies the creation of statements and collection letters:
- Generate statements/letters based on your own user-defined criteria
- Customize letters with bookmarks to import charge and patient information
- Build statements with a single click
- Created statements are routed to Patient Portal
- Generate a patient contact list
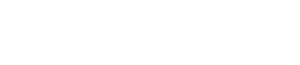
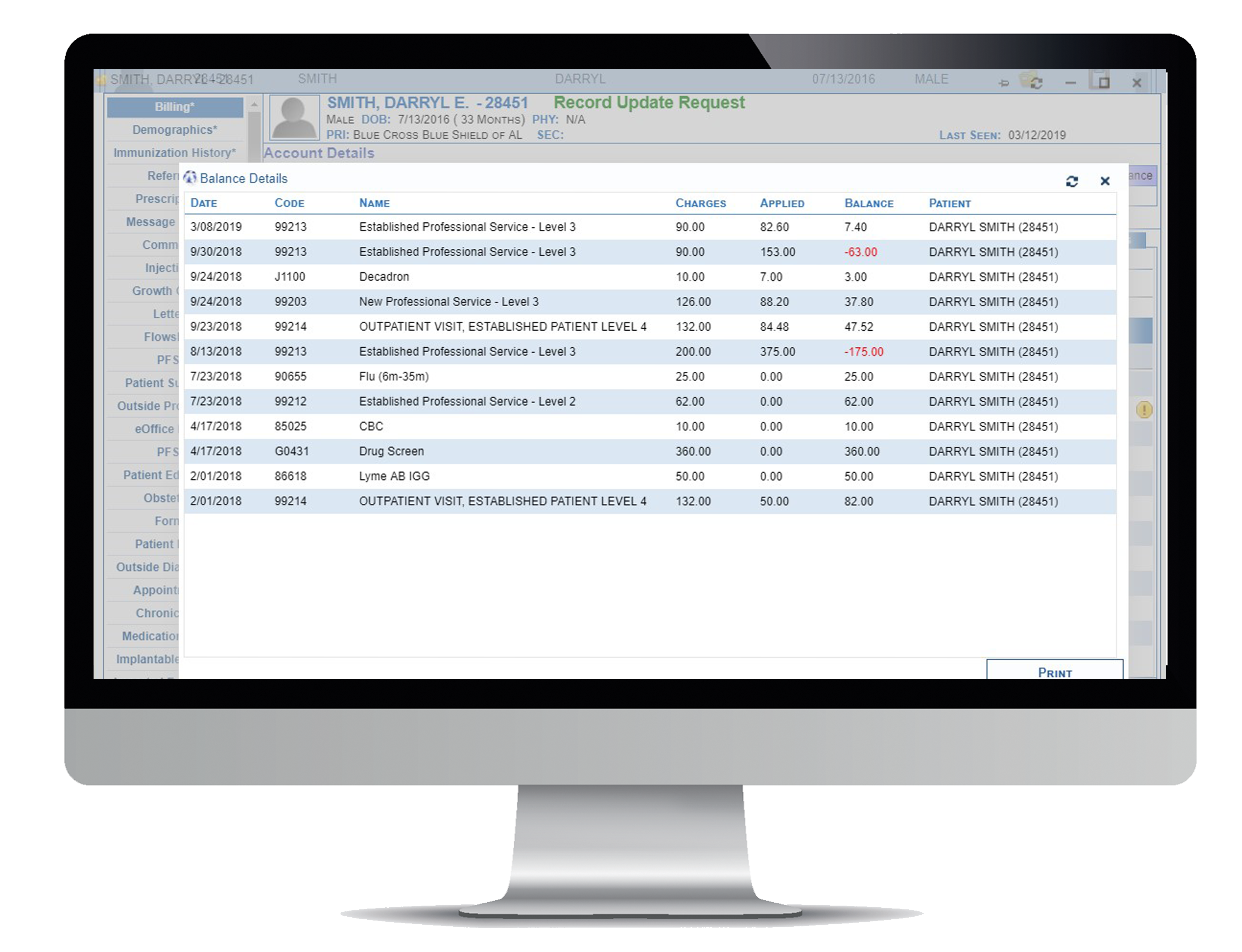
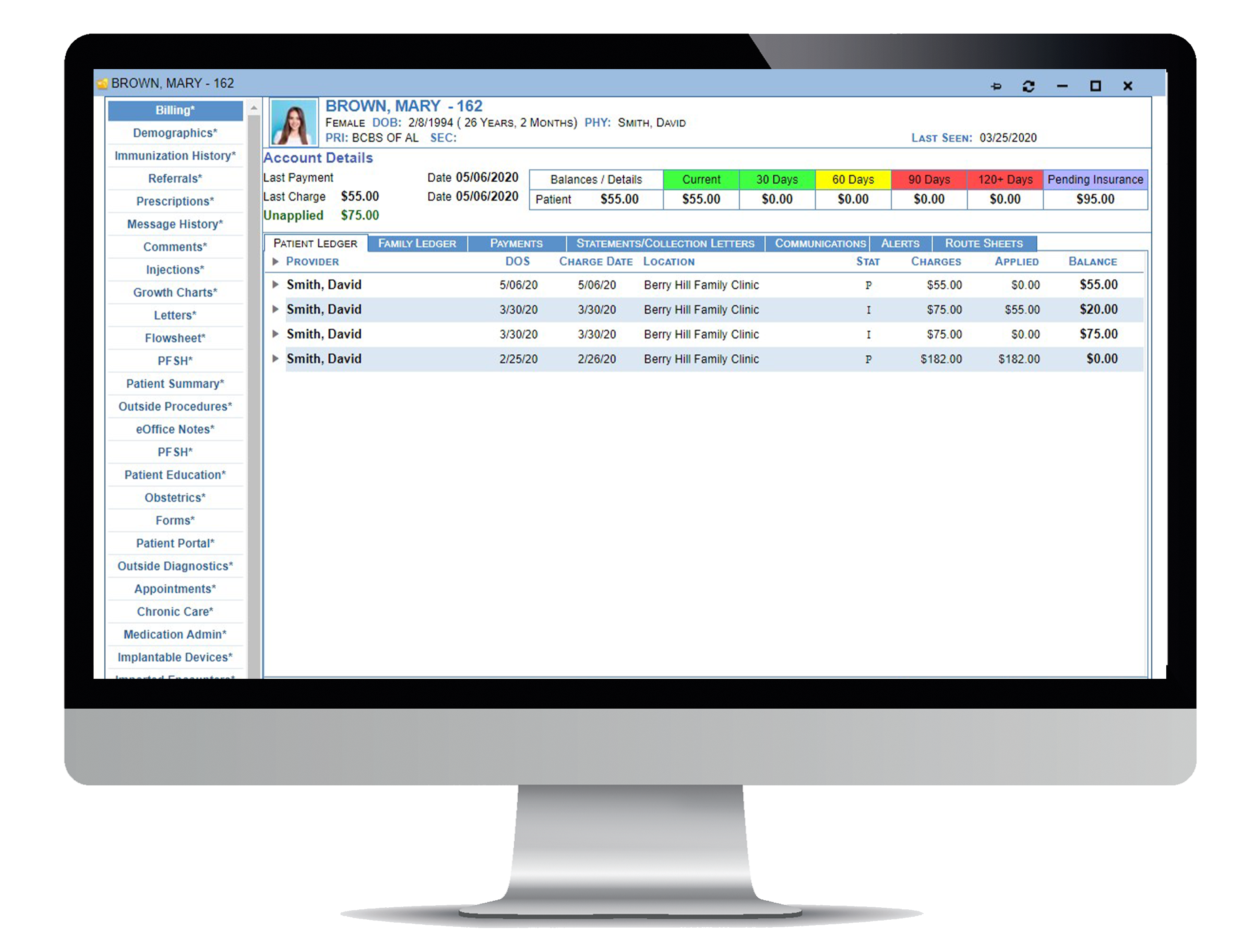
MedConnectHealth’s advanced reporting tools allow clients to quickly perform the following:
- Drill-down reporting to view summary and detailed transactions
- Access patient chart directly from financial reports
- Generate and review daily, weekly and monthly reports